Trying to Read the UK Cannabis Rulebook Without the Instructions
Buying cannabis oil and accessing medical cannabis sit under the same law, yet they rarely feel connected.
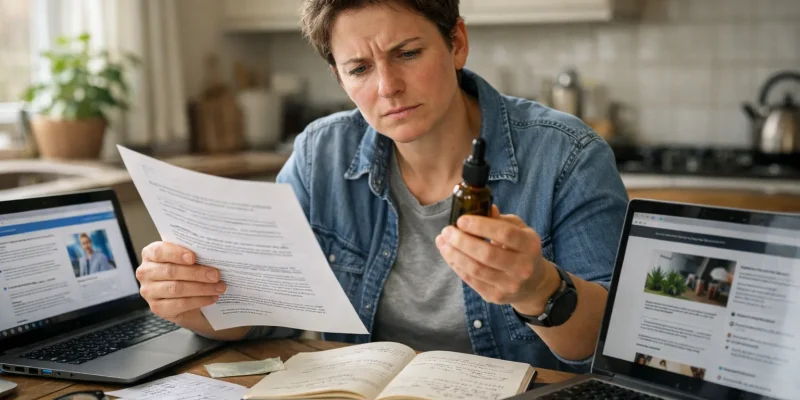
Information travels at different speeds depending on where you look. That mismatch leaves many people relying on partial answers, stitched together from reviews and clinical documentation that do not always meet.
The UK cannabis market is confusing for most people. Medical cannabis exists, but only through specialists, yet you can buy some cannabis oil without a prescription.
The rules are real, but they are not easy to find or understand. That gap leaves people trying to join the dots on their own.
Where Information Gaps Begin?

The first gap appears before any doctor is involved. People look online to understand what cannabis oil is and what options exist.
Most of what they find is not medical. It is based on products that are already being sold and discussed.
UK cannabis oil reviews pull those products together in one place so people can see what is on the market.
That kind of comparison does not replace clinical advice. It does explain why consumer information becomes the starting point for many people who are trying to make sense of a messy system.
Where Official Rules Add to the Confusion?
The next gap comes from how official information is published. Government guidance on medical cannabis exists, but it lives across policy pages and regulatory documents.
None of it is written for ease of access. It assumes time and familiarity with healthcare language.
The government’s own medicinal cannabis information and resources show how detailed that framework is.
It explains how prescribing works and who is allowed to make decisions. What it does not do is translate that structure into something easy to grasp at first pass. That distance between authority and accessibility is where confusion takes hold.
This is where speaking to a healthcare professional is recommended. Specialists are trained in these fields, and are there to help patients make informed and consensual decisions.
These are not decisions to take lightly, so medial advice should always be the firs port of call.
Why Evidence Does Not Always Settle the Question?
Another source of confusion comes from the evidence itself. Research on medical cannabis does exist, but it does not always give clear answers. Some studies point to benefit in limited cases.
Others show mixed results or gaps in data. That uncertainty filters down to patients, clinicians, and anyone trying to read up before making decisions.
A major evidence review published in the BMJ lays out those limits in plain terms. It shows where cannabis-based treatments may be considered and where caution still applies.
For a reader outside the medical world, that lack of certainty can feel frustrating. When evidence does not land cleanly, people tend to fill the space with opinion, experience, or marketing.
That gap is where bad information spreads. It is also where decent information gets misunderstood.
A quick skim can turn careful language into false confidence, which is exactly how mistakes start.
Fortunately, clearer pathways do exist for people who take the time to separate solid guidance from noise, even when the evidence itself feels unsettled.
Where Clinical Access Feels Like a Different World?
Medical cannabis runs on a different track. It is not about browsing shelves or comparing labels. It starts with appointments.
It moves through assessment. Decisions are made by specialists, with records kept and reviewed. That slower pace exists for a reason, even if it feels out of step with what people see online.
Cannabis clinics in the UK provide one of the few structured routes through that system.
They cut through the clutter to show how access works when it stays inside healthcare rather than retail, and is yet another reason to contact healthcare professionals for a consultation first.
For someone who began with product research, that reality check can feel abrupt. At the same time, it offers a clearer path than guesswork, especially when evidence and regulation do not always work hand in glove.
How Digital Access Changes Expectations?

Digital tools shape how people expect healthcare to work. Booking and tracking now feel like normal communication in many parts of the system. That changes patience levels.
It also changes how gaps in information stand out when services feel slow or unclear.
Health and care services already rely on digital access to bridge those gaps, as seen in the use of Android apps across Scottish health and care settings. When access improves in one area, it raises questions in others.
People start expecting the same clarity everywhere, including areas like medical cannabis where systems still feel fragmented.
Why the Gaps Keep Catching People Out?
None of this confusion comes from bad intent. It comes from systems that grew separately and never quite met in the middle.
Consumer information moves fast. Clinical systems move carefully. Official guidance moves slowly.
People end up caught between them, trying to make sense of rules, products, and pathways without a clear map.
Until those parts speak the same language, information gaps will keep shaping how the UK cannabis market is understood, often more than the law itself.





